NY Presbyterian Hospital - Cornell
Operative Report
Name: KO, KANG WEI
MRN: 02492702
ATT:
DICT: Brendon Stiles, M.D.
Admit Date:04/23/2012
Discharge Date:
Procedure Date:05/17/2012
SURGEON: Brendon Stiles, M.D.
CONSULTANT:
ASSISTANT:
PREOPERATIVE DIAGNOSIS: Bariatric surgery status post division of stomach with patient left in discontinuity.
POSTOPERATIVE DIAGNOSIS:
OPERATION: Esophagoscopy.
ANESTHESIA: Conscious sedation.
ANESTHESIOLOGIST: DR. NATALIA VASCHIA
BRIEF HISTORY:
Mr. Ko is a young man who had bariatric procedure which was complicated by postoperative bleeding necessitating division of his gastric pouch. He had been left in discontinuity. I had previously seen him and placed an esophagostomy drainage tube. I was asked to re-evaluate him today for quality of drainage and to make sure that his proximal gastric pouch was intact. The risks and benefits of the procedure were explained in detail to the patient. Written consent was obtained.
DESCRIPTION OF PROCEDURE:
The patient was brought to the operating room where conscious sedation was induced. He was continuously hemodynamically monitored. Once he was adequately sedated, a GIF upper endoscope was advanced through his oropharynx and down his esophagus. We were able to easily visualize the NG tube and the esophagostomy. These were fine. I followed the tube down to the distal esophagus and into the gastric pouch. The gastric pouch seemed to hold air fine and had no evidence of a leak. It looked healthy. I advanced the tube down to approximately 40 cm just above the GE junction. The pouch was exploited and the scope was carefully pulled back. I performed the entire
procedure.
DD:05/18/2012
DT:05/18/2012
Job:931328
Message Control: 931328
BRENDON STILES
ELECTRONICALLY SIGNED 5/26/2012 6:25
2012 - 2014 were the most difficult years of my life. In 2012, a routine gastric bypass surgery developed into life-threatening complications, several emergency surgeries, weeks spent intubated in the ICU, and months of hospital stay. It took almost 2 full years for me to recover. In 2014, I had an aortic valve replacement surgery. My chest was cracked open, my heart was stopped and put on bypass, then everything got put back together without any major issues.
Thursday, May 17, 2012
Saturday, May 5, 2012
Jenny's Update #2
Tony's surgery went well and is recovering smoothly. While he was drowsy after the surgery, he told me he just had a dream about transformer....he finds fun, as always. So no worries, that's the least thing I wish from all of you. He will be back on FB soon, I promise!
- Jenny Ko
- Jenny Ko
Wednesday, May 2, 2012
VAC Change & Abdomen Closure
Operative Note Summary
Patient: Kang Wei Ko
MRN: 2492702
Encounter Date: May 02, 2012
Operative Note:
SURGEON NAME: Francesco Rubino, MD [6739R]
PROCEDURE DATE:05/02/2012
ADMIT DATE:05/02/2012
PREOPERATIVE DIAGNOSIS: Discontinuity of GI Anatomy and Open Abdomen (Wound Vac) after Resection of Gastrojejunostomy for Endoluminal Bleed
POSTOPERATIVE DIAGNOSIS: Same
OPERATION: Abdominal Exploration and Washout; Closure of Abdomen with Alloderm + Wound Vac Placement + Esophageal Endoscopy and Cervical Esophagostomy Tube Placement
ATTENDING SURGEON: Francesco Rubino [6739R]
ATTENDING SURGEON: Brendon Stiles, MD
ASSISTANT SURGEON: Amanda Powers MD
The patient is a 35 yo male with morbid obesity, who underwent Roux en Y Gastric Bypass two months ago. He had two recurrent episodes of marginal ulcers with gastrointestinal bleeding successfully treated with endoscopic hemostasis. After a third recidivism of gastrointestinal bleeding last week with syncope he was admitted in critical conditions at another hospital in Queens. After a failed attempt to control GI bleed endoscopically, the patient underwent laparotomy with resection of gastro-jejunostomy and partial resection of gastric remnant. Gastrointestinal anatomy was left in discontinuity and the abdomen was left open due to edematous bowel. Last week the patient underwent abdominal exploration and washout with placement of feeding jejunostomy. The abdomen was left open due to significant edema of the viscera.
Patient's conditions and therapeutic plan have been discussed at length with his family, that consented for abdominal exploration, washout, abdominal closure, cervical esophagostomy, and possible reconstruction of gastrointestinal continuity.
PROCEDURE: The patient entered the operating room with orotracheal intubation. Following appropriate identification, he was placed in supine position on the operating table. Venodyne boots were applied. A surgical pause was performed in accordance with hospital regulations. Full general anesthesia was induced. The patient was prepped and draped in a supine position with appropriate padding and avoidance of hyper-extension of the extremities. Appropriate antibiotics were given intravenously.
Dr Stiles from thoracic surgery performed the left cervical esophagostomy with a 18F nasogastric tube on the left side of the esophagus (see his op note for details).
After removal of the Vac the abdominal cavity was washed copiously with saline. The position of the Jejunostomy tube was checked and was found to be securely in place in the Roux- limb. The JP drain was removed. The abdominal fascia was then separated from the subcutaneous tissue in a circumferential fashion leaving an edge of at least 2 cm. At this point the abdominal defect was evaluated and it was determined that it was not possible to close the abdominal wall safely. At this point the abdominal wall defect was measured. Then two pieces of Alloderm were assembled together appropriately to obtain a 32x20 cm mesh. This was secured to the fascial edges circumferentially with a running #1 Prolene suture. Then, white foam was placed against the alloderm and black foam layer was placedon top of the white foam. A KCI Vac was placed under suction to -100mmHg.The J tube was left to gravity.
Sterile dressings were applied. Anesthesia was well tolerated. The patient was left intubated and accompanied by the surgical team to the recovery room. Estimated blood loss was approximately 50cc. Sponge, needle and instrument counts were reported correct to the surgeon.
I was present during the entire procedure.
Francesco Rubino, MD [6739R]
(Electronic signature on file)
_____________________________________________
Note electronically signed by Francesco Rubino on Fri May 25, 2012 5:23 PM
Patient: Kang Wei Ko
MRN: 2492702
Encounter Date: May 02, 2012
Operative Note:
SURGEON NAME: Francesco Rubino, MD [6739R]
PROCEDURE DATE:05/02/2012
ADMIT DATE:05/02/2012
PREOPERATIVE DIAGNOSIS: Discontinuity of GI Anatomy and Open Abdomen (Wound Vac) after Resection of Gastrojejunostomy for Endoluminal Bleed
POSTOPERATIVE DIAGNOSIS: Same
OPERATION: Abdominal Exploration and Washout; Closure of Abdomen with Alloderm + Wound Vac Placement + Esophageal Endoscopy and Cervical Esophagostomy Tube Placement
ATTENDING SURGEON: Francesco Rubino [6739R]
ATTENDING SURGEON: Brendon Stiles, MD
ASSISTANT SURGEON: Amanda Powers MD
The patient is a 35 yo male with morbid obesity, who underwent Roux en Y Gastric Bypass two months ago. He had two recurrent episodes of marginal ulcers with gastrointestinal bleeding successfully treated with endoscopic hemostasis. After a third recidivism of gastrointestinal bleeding last week with syncope he was admitted in critical conditions at another hospital in Queens. After a failed attempt to control GI bleed endoscopically, the patient underwent laparotomy with resection of gastro-jejunostomy and partial resection of gastric remnant. Gastrointestinal anatomy was left in discontinuity and the abdomen was left open due to edematous bowel. Last week the patient underwent abdominal exploration and washout with placement of feeding jejunostomy. The abdomen was left open due to significant edema of the viscera.
Patient's conditions and therapeutic plan have been discussed at length with his family, that consented for abdominal exploration, washout, abdominal closure, cervical esophagostomy, and possible reconstruction of gastrointestinal continuity.
PROCEDURE: The patient entered the operating room with orotracheal intubation. Following appropriate identification, he was placed in supine position on the operating table. Venodyne boots were applied. A surgical pause was performed in accordance with hospital regulations. Full general anesthesia was induced. The patient was prepped and draped in a supine position with appropriate padding and avoidance of hyper-extension of the extremities. Appropriate antibiotics were given intravenously.
Dr Stiles from thoracic surgery performed the left cervical esophagostomy with a 18F nasogastric tube on the left side of the esophagus (see his op note for details).
After removal of the Vac the abdominal cavity was washed copiously with saline. The position of the Jejunostomy tube was checked and was found to be securely in place in the Roux- limb. The JP drain was removed. The abdominal fascia was then separated from the subcutaneous tissue in a circumferential fashion leaving an edge of at least 2 cm. At this point the abdominal defect was evaluated and it was determined that it was not possible to close the abdominal wall safely. At this point the abdominal wall defect was measured. Then two pieces of Alloderm were assembled together appropriately to obtain a 32x20 cm mesh. This was secured to the fascial edges circumferentially with a running #1 Prolene suture. Then, white foam was placed against the alloderm and black foam layer was placedon top of the white foam. A KCI Vac was placed under suction to -100mmHg.The J tube was left to gravity.
Sterile dressings were applied. Anesthesia was well tolerated. The patient was left intubated and accompanied by the surgical team to the recovery room. Estimated blood loss was approximately 50cc. Sponge, needle and instrument counts were reported correct to the surgeon.
I was present during the entire procedure.
Francesco Rubino, MD [6739R]
(Electronic signature on file)
_____________________________________________
Note electronically signed by Francesco Rubino on Fri May 25, 2012 5:23 PM
Esophagoscopy & Esophagostomy
NY Presbyterian Hospital - Cornell
Operative Report
Name: KO, KANG WEI
MRN: 02492702
ATT:
DICT: Brendon Stiles, M.D.
Admit Date:04/23/2012
Discharge Date:
Procedure Date:05/02/2012
SURGEON: Brendon Stiles, M.D.
CONSULTANT:
ASSISTANT: DR. MICHAEL NAZERIAN
PREOPERATIVE DIAGNOSIS: Bariatric surgery with postoperative bleeding requiring partial gastrectomy and esophagus left in discontinuity.
POSTOPERATIVE DIAGNOSIS:
OPERATION: 1. Esophagoscopy. 2. Esophagostomy tube via cervical incision.
ANESTHESIA: General endotracheal anesthesia.
ANESTHESIOLOGIST:
BRIEF HISTORY:
Mr. Ko is a young male who underwent gastric bypass surgery. Postoperative course was complicated by bleeding and exploration at an outside hospital at which time a partial gastrectomy was performed. The patient was left in discontinuity. I had previously performed an endoscopy to ensure that he had a well-healing upper stomach. At that time we noted an approximately 2-3 cm proximal gastric pouch that looked fine. We elected to wait for more definitive procedures at that instance. He was brought back to the operating room today hopefully for abdominal closure by Dr. Rubino's team. I was also asked to re-evaluate him to place a more definitive esophageal drain. We had discussed the option of diverting him, but I did not want to leave a long segment of stomach and the upper gastric pouch in discontinuity for fear that we would have no where to drain and that it would rupture. Although I had described to the family that even with tube drainage there was some risk of rupture, I deemed this to be a safer operation than leaving the entire tracking complete discontinuity without drainage. I therefore recommended a cervical esophagostomy tube. The risks and benefits of this were described and written consent was obtained.
DESCRIPTION OF PROCEDURE:
The patient was brought to the operating room, placed supine upon the operating room table. I performed an esophagoscopy first. The esophagus looked good and healthy. The GE junction was approximately 40 cm. Distal to that there was approximately 2-3 cm of gastric remnant. This appeared to be well healed without evidence of leak. The entire thing was well drained with the existing NG tube. The scope was then pulled back and removed. At this point Dr. Rubino's was in the operating room too. We prepped the whole field as one going from the chin down to the pelvis. He began work on the abdomen, which will be dictated separately. I had extended the neck and made a left transverse cervical incision. Underlying platysma and subcutaneous tissue was cauterized. Sternocleidomastoid was identified and retracted laterally. Carotid sheath and its contents were mobilized laterally as well. The thyroid vein was divided, exposed the tracheoesophageal junction. I dissected bluntly behind the esophagus freeing it up from its posterior attachments to vertebral bodies. I then bluntly and circumferentially dissected it taking care to stay close to the wall of the esophagus rather than the trachea. A Penrose drain was placed around it and the esophagus was mobilized both proximally and distally. It was then pulled up into view. The NG tube was removed. I placed a pursestring suture around the left lateral wall of the esophagus. A small esophagostomy was made and enlarged slightly. An 18-French NG tube was passed through a small counter incision in the skin and then through the esophagostomy and down into the distal esophagus. It was fixed in place with the pursestring suture. A repeat esophagostomy was performed. Demonstrated no evidence of stricturing of the esophagus with the pursestring and it showed that the NG tube was in good position. The scope was then pulled back. Incision was closed with layers of absorbable suture disclosing the platysma and the skin. Drain was fixed in place with a simple drain stitch. I was present and performed this entire part of the operation. The rest will be dictated separately by Dr. Rubino.
DD:05/02/2012
DT:05/02/2012
Job:395270
Message Control: 395270
BRENDON STILES
ELECTRONICALLY SIGNED 5/9/2012 8:19
Operative Report
Name: KO, KANG WEI
MRN: 02492702
ATT:
DICT: Brendon Stiles, M.D.
Admit Date:04/23/2012
Discharge Date:
Procedure Date:05/02/2012
SURGEON: Brendon Stiles, M.D.
CONSULTANT:
ASSISTANT: DR. MICHAEL NAZERIAN
PREOPERATIVE DIAGNOSIS: Bariatric surgery with postoperative bleeding requiring partial gastrectomy and esophagus left in discontinuity.
POSTOPERATIVE DIAGNOSIS:
OPERATION: 1. Esophagoscopy. 2. Esophagostomy tube via cervical incision.
ANESTHESIA: General endotracheal anesthesia.
ANESTHESIOLOGIST:
BRIEF HISTORY:
Mr. Ko is a young male who underwent gastric bypass surgery. Postoperative course was complicated by bleeding and exploration at an outside hospital at which time a partial gastrectomy was performed. The patient was left in discontinuity. I had previously performed an endoscopy to ensure that he had a well-healing upper stomach. At that time we noted an approximately 2-3 cm proximal gastric pouch that looked fine. We elected to wait for more definitive procedures at that instance. He was brought back to the operating room today hopefully for abdominal closure by Dr. Rubino's team. I was also asked to re-evaluate him to place a more definitive esophageal drain. We had discussed the option of diverting him, but I did not want to leave a long segment of stomach and the upper gastric pouch in discontinuity for fear that we would have no where to drain and that it would rupture. Although I had described to the family that even with tube drainage there was some risk of rupture, I deemed this to be a safer operation than leaving the entire tracking complete discontinuity without drainage. I therefore recommended a cervical esophagostomy tube. The risks and benefits of this were described and written consent was obtained.
DESCRIPTION OF PROCEDURE:
The patient was brought to the operating room, placed supine upon the operating room table. I performed an esophagoscopy first. The esophagus looked good and healthy. The GE junction was approximately 40 cm. Distal to that there was approximately 2-3 cm of gastric remnant. This appeared to be well healed without evidence of leak. The entire thing was well drained with the existing NG tube. The scope was then pulled back and removed. At this point Dr. Rubino's was in the operating room too. We prepped the whole field as one going from the chin down to the pelvis. He began work on the abdomen, which will be dictated separately. I had extended the neck and made a left transverse cervical incision. Underlying platysma and subcutaneous tissue was cauterized. Sternocleidomastoid was identified and retracted laterally. Carotid sheath and its contents were mobilized laterally as well. The thyroid vein was divided, exposed the tracheoesophageal junction. I dissected bluntly behind the esophagus freeing it up from its posterior attachments to vertebral bodies. I then bluntly and circumferentially dissected it taking care to stay close to the wall of the esophagus rather than the trachea. A Penrose drain was placed around it and the esophagus was mobilized both proximally and distally. It was then pulled up into view. The NG tube was removed. I placed a pursestring suture around the left lateral wall of the esophagus. A small esophagostomy was made and enlarged slightly. An 18-French NG tube was passed through a small counter incision in the skin and then through the esophagostomy and down into the distal esophagus. It was fixed in place with the pursestring suture. A repeat esophagostomy was performed. Demonstrated no evidence of stricturing of the esophagus with the pursestring and it showed that the NG tube was in good position. The scope was then pulled back. Incision was closed with layers of absorbable suture disclosing the platysma and the skin. Drain was fixed in place with a simple drain stitch. I was present and performed this entire part of the operation. The rest will be dictated separately by Dr. Rubino.
DD:05/02/2012
DT:05/02/2012
Job:395270
Message Control: 395270
BRENDON STILES
ELECTRONICALLY SIGNED 5/9/2012 8:19
Tuesday, May 1, 2012
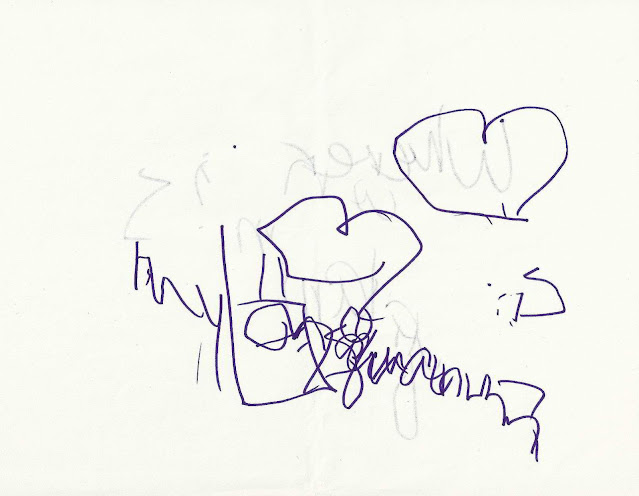
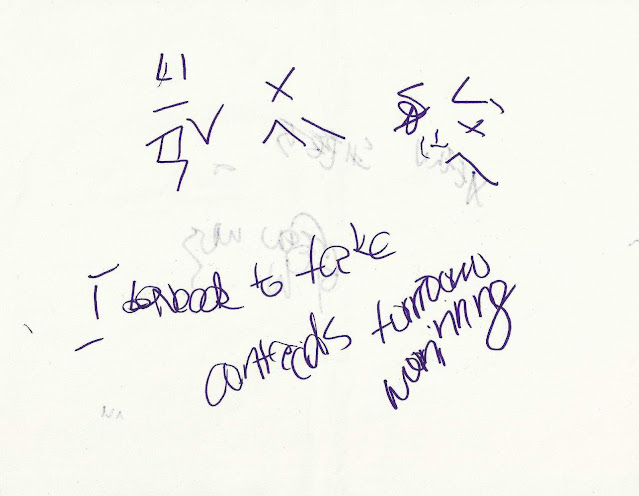
Hospital Scribbling
For a period of 2 weeks, due to the severity of my internal injuries, I was intubated, heavily medicated, in a great deal of pain, completely confused about all that was happening around me and TO me, yet not being able to speak.
As I drifted in and out of consciousness, I attempted to communicate with my loved ones by desperately trying to write down what I wanted to say. I thought I was writing in a clear and concise manner as I have always written...but I was thoroughly shocked later on to discover just what I was actually writing/scribbling:
Subscribe to:
Posts (Atom)